At a recent round table with HR leaders, one theme kept surfacing: we all know “trauma-informed workplaces” are important, but many fear they could get it wrong.
Managers worry about overstepping; HR wonders how to support leaders without expecting them to act like therapists.
This guide is intended to bridge that gap. It equips HR and managers with language, frameworks and practices rooted in research and lived experience, drawing also from international and Australian sources on trauma-informed approach.
NOTE: this is not a replacement for getting the right help and support, this is here to get the conversation started.
The prevalence of trauma and how trauma shows up at work
Before diving into processes, it’s essential to understand how common trauma is, and how it shows up in the workplace:
- Up to 75% of Australian adults have experienced at least one traumatic event in their life.
- Between 57% and 75% of Australians will experience some form of trauma in their lifetime.
- Poor mental health costs the Australian economy AUD $6M per year in lost productivity.
- In many workplaces, stressors like bullying, discrimination, or chronic pressure act as “microtraumas” (or known at little t) that compound over time.
When a person carries trauma, past or present, it can affect memory, focus, emotional regulation, interpersonal trust, and how safe they feel in their work environment. Some may “mask” this well, so trauma doesn’t always look obvious.
This is why a trauma-informed workplace is not something we can ignore anymore. It is everywhere.
Big T & Little t: what does it mean?
One of the most useful distinctions managers and HR can hold is between Big T and little t trauma:
- Big T Trauma: Major events such as abuse, accidents, war, natural disasters—things widely considered “traumatic.”
- Little t Trauma: Cumulative, repeated stressors, microaggressions, exclusion, unresolved conflict, chronic uncertainty.
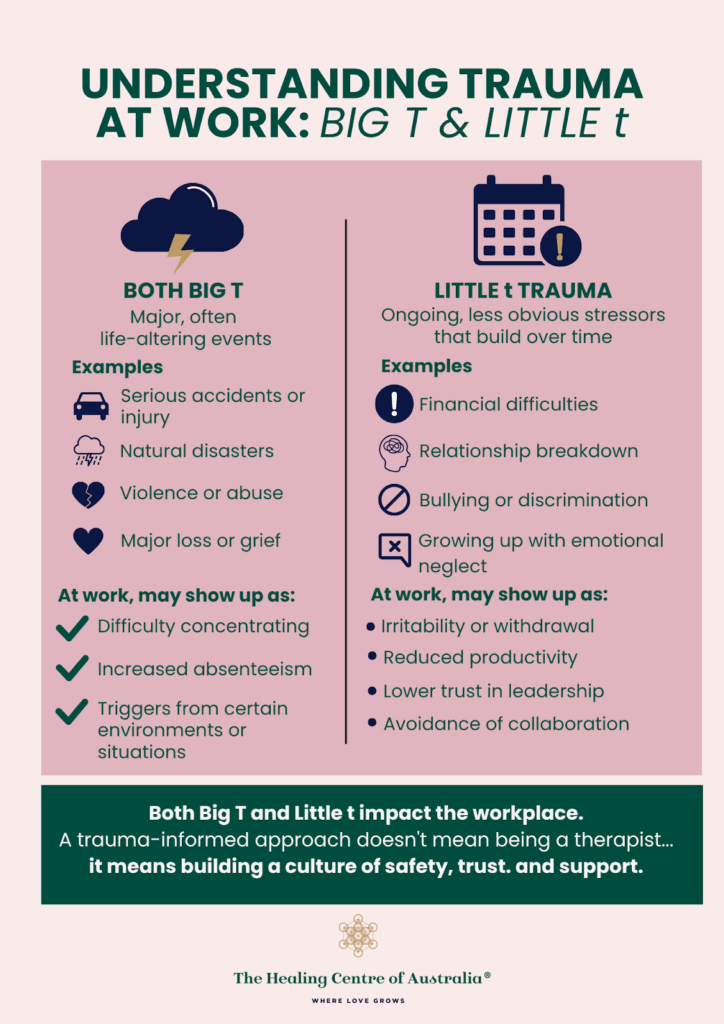
While Big T can be more noticeable, “little t” events can erode wellbeing over time. People may bring both kinds of trauma into work. Recognising that trauma isn’t always a single dramatic event helps remove stigma and opens the space for more empathetic responses.
Principles of Trauma-Informed Workplaces
Drawing from the Australian Human Rights Commission guidelines, Mentally Healthy Workplaces, and other frameworks, the following principles are foundational.
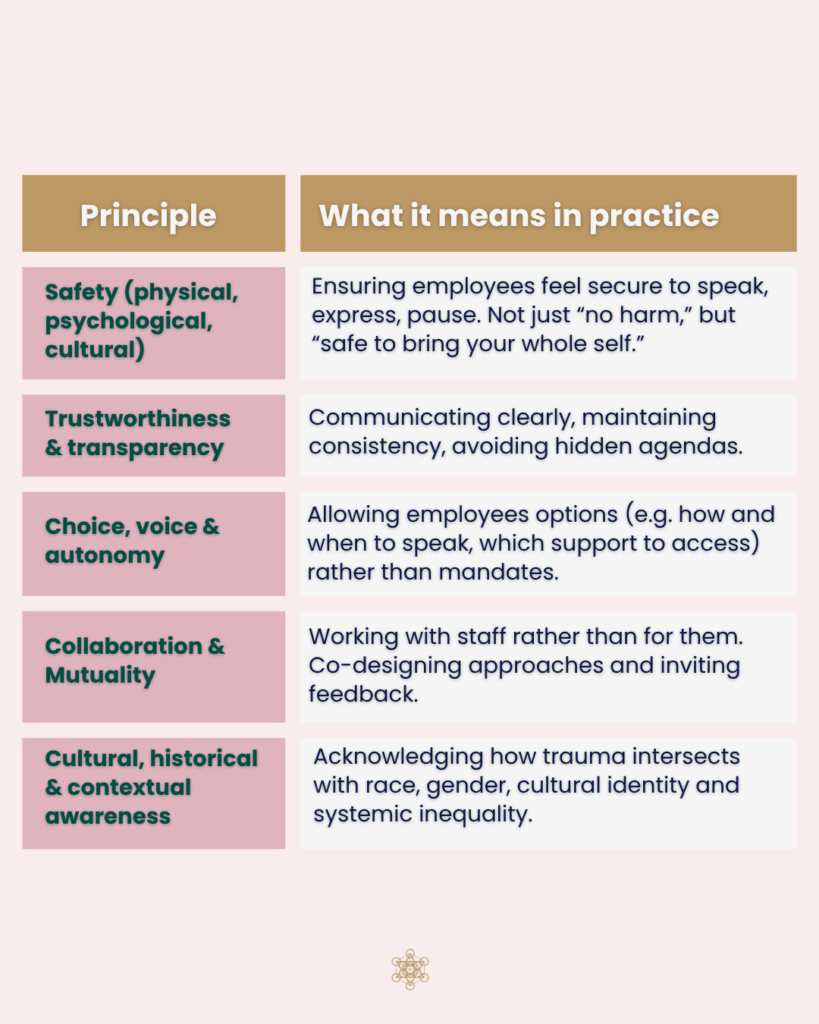
Embedding these is not a “checklist” exercise. It requires ongoing commitment, reflection, and iteration.
Supporting managers to lead well
One of the key insights from our round table was this: HR can’t just “know” trauma-informed practice, they must support managers to apply it. Here’s how:
1. Provide framing, language & scripts
Managers often hesitate because they don’t know what to say. Equip them with:
- Opening phrases: “I’ve noticed some challenges lately, and I’m here to support you if you’d like to talk”
- Listening prompts: “Would you like to share what feels difficult right now?”
- Referral language: “You’re not alone, here are some support options (HR, EAP, etc.).”
Include “dos and don’ts” (e.g. avoid judgmental or dismissive responses). The Australian HR Institute’s trauma-informed HR practices emphasise using neutral, respectful language in documentation and communications.
2. Clarify when to hold & when to refer
Managers can’t, and shouldn’t, carry therapeutic burdens. Part of this training is defining boundaries:
- Hold space (listen, validate, ask how you can support)
- Refer onward (HR, EAP, external clinicians)
- Know that asking someone if they’d like to talk is not therapy
As stated by Worksafe Queensland guidelines trauma-informed return-to-work processes: “This approach is not about being a therapist. It’s about taking a human approach… creating a safe space for recovery.”
3. Build psychological safety at team level
Managers can embed trauma-informed principles in their daily interactions:
- Normalise pauses or check-ins
- Encourage vulnerability (leader models: “I’m having a tough day too”)
- Invite feedback on workload, process, support
- Create space for team debrief or reflection
Psychological safety has been shown to be more predictive of high-performing teams than any other factor.
4. Use Trauma-Informed policies & HR processes
Managers should not act alone, HR must rewrite policy, process and structure through a trauma lens. This includes:
- Flexible working, gradual adjustments, safe reporting channels
- Grievance / harassment procedures designed to minimise retraumatisation (e.g. fewer repeated recountings, consent to retell, varied formats)
- Performance or disciplinary frameworks that account for mental health context
- Embedding trauma-informed language in documentation and role descriptions (avoiding language like “claim,” “complain,” or “accused”)
- EAP support for all team members (making this known as much as possibel)
By doing this, managers have structural support rather than being the “sole buffer.”
Example of a Trauma-Informed Workplace (fictional)
A manager sees an employee, beginning to take more time off, withdrawing in meetings, and missing deadlines. Rather than waiting until things escalate, they initiated a one-on-one:
“Jessica, I’ve noticed some changes in your workload and presence, no judgments. I want to check in: how are you doing, and is there a way I can support you? If you prefer, we can talk about options or adjustments.”
Jessica didn’t share trauma immediately, but did say she’d been managing stress at home. The manager responded with validation (“That sounds incredibly heavy”) and offered possibilities, reduced deadlines for a fortnight, connecting to HR for options, and letting Jessica choose how she wanted to talk further.
That conversation built trust, prevented escalation, and allowed Jessica to feel seen, and it didn’t require the manager to act as a counsellor.
What HR should track
To ensure lasting impact, HR should monitor outcomes. Suggested metrics include:
- Employee engagement / safety survey scores (specifically on trust, psychological safety)
- Uptake of support services (EAP, coaching, wellbeing programs)
- Absenteeism, turnover, retention rates
- Feedback on manager training (confidence, comfort in conversations)
- Qualitative feedback: “Do you feel safe to share challenges?”
Trauma-informed organisational change is iterative. Use surveys and feedback loops to refine practices over time.
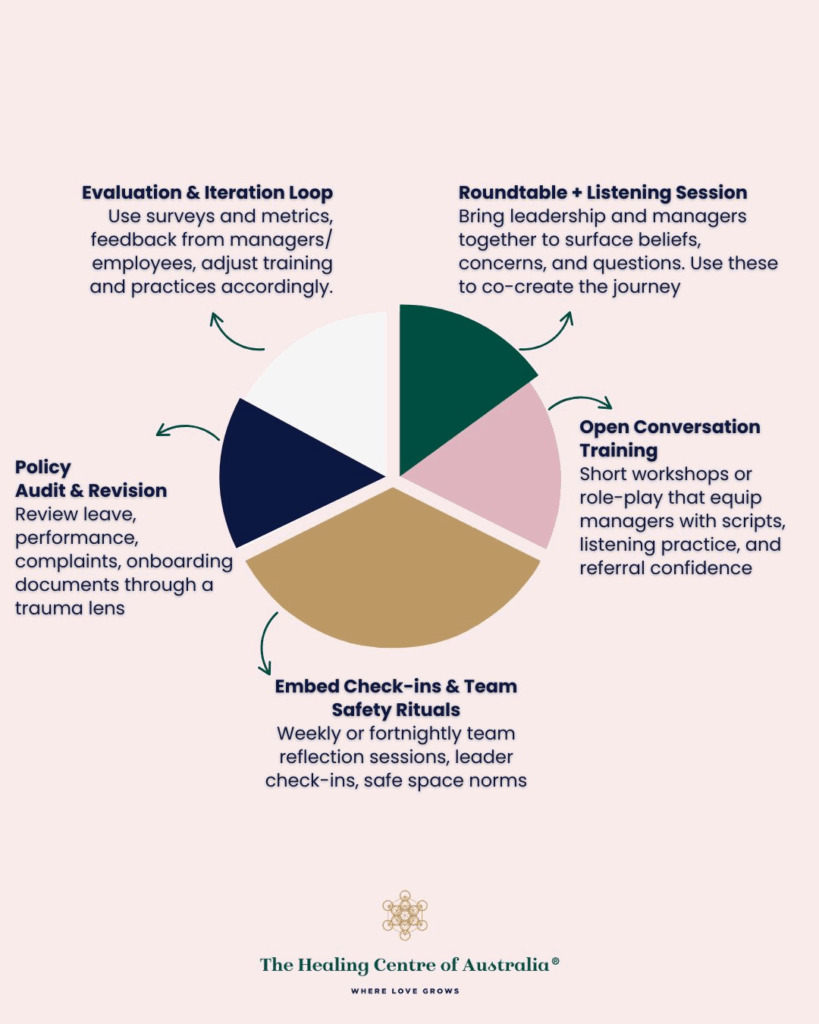
5 practical steps to help HR & Leadership be more wellbeing centric
1. Roundtable + Listening Session
Bring leadership and managers together to surface beliefs, fears, and questions. Use these to co-create the journey.
2. Trauma-Informed Conversation Training
Short workshops or role-play that equip managers with scripts, listening practice, and referral confidence.
3. Policy Audit & Revision
Review leave, performance, complaints, onboarding documents through a trauma lens (safety, language, flexibility).
4. Embed Check-ins & Team Safety Rituals
Weekly or fortnightly team reflection sessions, leader check-ins, safe space norms.
5. Evaluation & Iteration Loop
Use surveys and metrics; feedback from managers/employees; adjust training and practices accordingly.
From awareness to practice – start now
HR does not need to wait for perfect conditions to begin. As the round table affirmed, nobody wants to get it wrong, but waiting often means harm goes unaddressed.
By shifting power, providing structure, and equipping managers with care (not clinical burden), organisations can move from well-intended rhetoric to trauma-informed practice.
If you’re ready to begin, you don’t need clinical expertise, just curiosity, humility, and a commitment. Over time, the small changes add up: healthier teams, more trust, and a workplace where everyone can bring their whole selves.
